Cardiovascular | Electrophysiology | Intrinsic Cardiac Conduction System
TLDRThis educational video script delves into the fascinating world of electrophysiology, focusing on the heart's unique ability to self-regulate through a process known as automaticity. It explains how the heart's intrinsic pacemaker cells, such as the sinoatrial (SA) node, generate the rhythmic contractions without external nervous system input. The script explores the conduction system of the heart, detailing the path from the SA node through the atrioventricular (AV) node, bundle of His, and Purkinje fibers, which ensures the heart's coordinated beating. Furthermore, it breaks down the cellular processes of depolarization and repolarization, highlighting the role of various ion channels and the significance of the sarcoplasmic reticulum in muscle contraction. The script promises a continuation in part two, where it will discuss the extrinsic factors like the sympathetic and parasympathetic nervous systems that can modulate the heart's intrinsic rhythm.
Takeaways
- 💓 **Automaticity of the Heart**: The heart has an intrinsic ability to spontaneously depolarize itself, generating action potentials that spread throughout the myocardium, triggering contraction without relying on the nervous system.
- 🌀 **Cardiac Conduction System**: The heart's conduction system includes the SA node, AV node, Bundle of His, and Purkinje fibers, which are responsible for initiating and coordinating heartbeats.
- 🔵 **SA Node as Pacemaker**: The sinoatrial (SA) node, located in the right atrium, is the primary pacemaker of the heart, setting the baseline heart rate between 60 to 80 beats per minute.
- 🚦 **AV Node Delay**: The atrioventricular (AV) node introduces a 0.1-second delay, allowing the atria to contract and push blood into the ventricles before the ventricles contract.
- 🤝 **Gap Junctions and Desmosomes**: These cellular structures allow for the passage of ions between cells and keep cardiac muscle cells tightly connected, enabling the synchronized contraction of the heart.
- 🔋 **Role of Calcium**: Calcium ions play a crucial role in the contraction of cardiac muscle cells. The influx of calcium through various channels leads to the formation of cross-bridges between actin and myosin, resulting in muscle contraction.
- 🔁 **Repolarization**: After depolarization, potassium channels open, allowing potassium ions to leave the cell, which helps to repolarize the cell and return it to its resting membrane potential.
- ⚡ **Action Potentials**: The flow of sodium and calcium ions through voltage-gated channels generates action potentials in nodal cells, which then spread to contractile cells via Gap Junctions.
- 🤖 **Excitation-Contraction Coupling**: The process by which an electrical stimulus (action potential) leads to a mechanical response (contraction) in cardiac cells is known as excitation-contraction coupling.
- 🧵 **Sarcoplasmic Reticulum**: This specialized structure in cardiac cells stores and releases calcium ions, regulating the contraction and relaxation cycle of the heart.
- 🔄 **Calcium Regulation**: Proper heart function depends on the tight regulation of calcium ions, which must be sequestered in the sarcoplasmic reticulum and released when needed for contraction.
Q & A
What is the intrinsic ability of the heart called?
-The intrinsic ability of the heart is called automaticity, which is the heart's ability to spontaneously depolarize itself and trigger action potentials without relying on the nervous system.
What are the two types of cells found in the myocardium?
-The two types of cells found in the myocardium are nodal cells, which are non-contractile and generate automaticity, and contractile cells, which contain the contractile proteins and are responsible for the actual contraction of the heart.
What is the role of the SA node in the heart?
-The SA node, or sinoatrial node, acts as the heart's natural pacemaker. It is responsible for setting the heart rate by generating action potentials that spread throughout the atria, initiating the heartbeat.
What is the significance of the 0.1-second delay at the AV node?
-The 0.1-second delay at the AV node allows the atria to contract and push blood into the ventricles before the ventricles contract. This ensures efficient blood flow from the atria to the ventricles and prevents simultaneous contraction of the atria and ventricles.
How do the action potentials from the SA node reach the left atrium?
-The action potentials from the SA node reach the left atrium via the Bachman's bundle, a specialized structure that connects the SA node in the right atrium to the left atrium.
What are the components of the cardiac conduction system?
-The components of the cardiac conduction system include the SA node, internodal pathways, Bachman's bundle, AV node, bundle of His, right and left bundle branches, and Purkinje fibers.
What are the 'funny' sodium channels in nodal cells?
-The 'funny' sodium channels in nodal cells are unique because they are leaky, allowing a slow influx of sodium ions into the cell. This slow depolarization is part of the mechanism that allows the heart to generate its own rhythm.
How do T-type calcium channels contribute to the depolarization of nodal cells?
-T-type calcium channels open when the membrane potential reaches around -55 millivolts. As these channels open, calcium ions flow into the cell, further depolarizing the membrane and contributing to the generation of an action potential.
What is the role of L-type calcium channels in the action potential of nodal cells?
-L-type calcium channels open when the membrane potential reaches the threshold potential of around -40 millivolts. The influx of calcium ions through these channels causes a rapid depolarization, leading to the peak of the action potential.
How do desmosomes and gap junctions work together in cardiac cells?
-Desmosomes provide structural support and keep cardiac cells tightly connected, while gap junctions allow for the rapid spread of electrical signals between cells. Together, they form intercalated discs, which are crucial for the synchronized contraction of the heart.
What is the functional unit of cardiac muscle contraction?
-The functional unit of cardiac muscle contraction is known as the functional syncytium. It refers to the synchronized contraction of cardiac muscle cells due to their interconnectedness via gap junctions, which allows the heart to contract as a single unit.
Outlines
😀 Introduction to Electrophysiology and the Heart's Automaticity
The video begins with an introduction to electrophysiology, emphasizing the heart's unique ability to depolarize itself without reliance on the nervous system. The concept of automaticity is introduced, which is the heart's intrinsic capability to spontaneously depolarize and trigger action potentials throughout the myocardium, leading to contraction. The presenter outlines the structure of the heart, highlighting the distinction between nodal cells, responsible for generating automaticity, and contractile cells, which actually carry out the contraction. The SA node, located in the right atrium, is identified as the primary pacemaker of the heart, initiating the sinus rhythm.
🔄 The Cardiac Conduction System and the Role of the SA Node
The SA node's function as the heart's pacemaker is explored, detailing how it sets the sinus rhythm at approximately 60 to 80 beats per minute. The video explains the normal conduction pathway of electrical impulses from the SA node through the atria via the Bachman's bundle and internodal pathways to the AV node. The importance of the 0.1-second delay at the AV node is discussed, which allows the atria to contract and push blood into the ventricles before the ventricles contract.
🚏 The Path from the AV Node to the Bundle Branches
Following the AV node's role, the video describes the conduction of electrical impulses through the bundle of His, which then splits into the right and left bundle branches. These branches further divide into Purkinje fibers, which are responsible for activating different parts of the myocardium. The video recaps the sequence of the cardiac conduction system, from the SA node to the AV node, then to the bundle of His, and finally to the bundle branches and Purkinje fibers.
🌐 Cell-to-Cell Communication and the Generation of Action Potentials
The video delves into the cellular mechanisms of action potential generation, focusing on the communication between nodal cells and contractile cells through gap junctions. It explains the role of 'funny sodium channels' in nodal cells, which allow a slow influx of sodium ions, leading to depolarization. The opening of T-type calcium channels and the subsequent influx of calcium ions are also discussed, highlighting how these ions work together to depolarize the cell and trigger an action potential.
🛠️ The Role of Calcium and Potassium Channels in Cell Depolarization
The video continues to describe the process of depolarization, emphasizing the role of L-type calcium channels that open once the threshold potential is reached, leading to a rapid influx of calcium ions. The subsequent rise in positive charge inside the cell is detailed, along with the impact on the contractile cell through gap junctions. The structural proteins, like connexins and desmosomes, that keep cells tightly connected are also explained, ensuring the synchronized contraction of the heart muscle.
🔗 Gap Junctions and Desmosomes in Cardiac Cell Synchronization
The concept of intercalated discs, formed by the combination of gap junctions and desmosomes, is introduced as a key structural component for cardiac cell synchronization. The video explains how the influx of cations through gap junctions into the contractile cell raises the membrane potential towards the threshold, triggering the opening of voltage-gated sodium channels and initiating an action potential. The different resting and threshold potentials in various cells are also discussed.
🔋 The Plateau Phase and Calcium-Induced Calcium Release
The video describes the plateau phase of the cardiac action potential, during which calcium ions continue to enter the cell while potassium ions exit, maintaining the depolarized state. It explains the concept of calcium-induced calcium release, where the influx of calcium ions triggers the release of more calcium from the sarcoplasmic reticulum, leading to muscle contraction. The role of T-tubules and the proteins involved in this process, such as calmodulin and ryanodine receptors, are also detailed.
🤝 The Functional Syncytium and Cardiac Muscle Contraction
The video discusses the functional syncytium, a network of interconnected cardiac muscle cells that contract in unison due to gap junctions. It explains how the binding of calcium to troponin changes the shape of the troponin-tropomyosin complex, allowing myosin to interact with actin and form cross-bridges, which leads to muscle contraction. The importance of synchronized contraction for efficient heart function is emphasized.
🔙 Repolarization and Restoring Calcium Balance
The final phase of the action potential is described, focusing on repolarization and the restoration of calcium balance. The video explains how L-type calcium channels close and potassium channels open, leading to the efflux of potassium ions and a return to the resting membrane potential. The mechanisms for calcium resequestration into the sarcoplasmic reticulum and extracellular environment are detailed, including the use of ATP and the role of sodium-calcium exchangers.
🔄 Resting Membrane Potential and the Onset of the Next Action Potential
The video concludes with a discussion of the resting membrane potential and the factors that maintain it until the next action potential is triggered. It explains the gradual closure of potassium channels and the opening of sodium channels, which allows sodium ions to leak into the cell and raise the membrane potential towards the threshold. The anticipation of part two, which will explore the extrinsic factors affecting heart rate, is also mentioned.
Mindmap
Keywords
💡Electrophysiology
💡Automaticity
💡Sinoatrial Node (SA Node)
💡Action Potentials
💡Nodal Cells
💡Contractile Cells
💡Atrioventricular Node (AV Node)
💡Bundle of His
💡Gap Junctions
💡Sarcoplasmic Reticulum
💡Tropomyosin and Troponin
Highlights
The heart has the intrinsic ability to spontaneously depolarize itself, a characteristic known as automaticity.
Automaticity allows the heart to generate action potentials without dependence on the nervous system.
The sinoatrial node (SA node) is the primary pacemaker of the heart, setting the heart's rhythm.
The SA node is located in the right atrium and is responsible for initiating the heartbeat.
The atrioventricular node (AV node) acts as a bridge between the atria and ventricles, introducing a delay crucial for efficient heart function.
The bundle of His and bundle branches are essential components for the propagation of electrical signals throughout the heart.
The myocardium is composed of nodal cells, which generate automaticity, and contractile cells, which are responsible for the heart's contraction.
The sarcoplasmic reticulum plays a key role in calcium regulation, enabling and terminating muscle contraction.
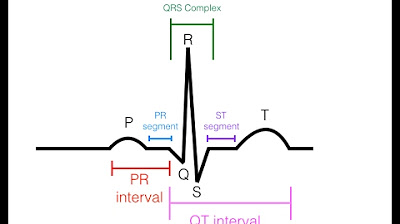
The electrophysiological process of the heart involves phases 0 to 4, detailing the movement of ions across cell membranes.
Gap junctions between cardiac cells allow for rapid and synchronized contraction, forming a functional syncytium.
The resting membrane potential and threshold potential vary between nodal and contractile cells, influencing the initiation of action potentials.
The repolarization phase of the cardiac action potential is primarily driven by the efflux of potassium ions.
The autonomic nervous system, including sympathetic and parasympathetic components, can modulate the intrinsic heart rate.
The heart's conduction system ensures the proper timing and coordination of atrial and ventricular contractions for optimal cardiac output.
Calcium ions are central to the excitation-contraction coupling in cardiac cells, leading to muscle contraction.
Desmosomes provide structural support and maintain the integrity of cardiac cells, allowing for effective cell-to-cell communication.
The video concludes with a preview of part two, which will delve into the extrinsic factors affecting heart rate and rhythm.
Transcripts
Browse More Related Video
EKG/ECG Interpretation (Basic) : Easy and Simple!
EKG Basics | How to Read & Interpret EKGs: Updated Lecture

Cardiovascular | Cardiac Cycle

Coronary circulation of the heart

Circulatory System and Pathway of Blood Through the Heart

Sinus Bradycardia ECG/EKG Interpretation, Causes, Treatment, Nursing NCLEX Review Cardiac
5.0 / 5 (0 votes)
Thanks for rating: