Diagnostic Testing Accuracy
TLDRThis video script delves into the importance of diagnostic testing in clinical practice, emphasizing how tests clarify symptom causes, support treatment decisions, and assess disease progression. It introduces the concept of pre-test probability, illustrated with a case study on pulmonary embolism. The script explains diagnostic parameters like sensitivity, specificity, predictive values, and accuracy, highlighting their roles in confirming or ruling out diseases. The example of a D-dimer test underscores the clinical implications of these parameters, ultimately guiding the doctor to rule out pulmonary embolism in a patient presenting with chest pain and shortness of breath.
Takeaways
- 🧠 Understanding diagnostic tests is crucial for interpreting clinical data and making informed therapeutic decisions.
- 🩺 The purpose of clinical tests includes clarifying symptoms' causes, assessing disease severity, prognosis, monitoring disease progression, and therapy response.
- 📊 Diagnostic tests can be performed in parallel or sequentially, with sequential testing guided by the results of previous tests.
- 🤔 Pre-test probability is the likelihood of a disease being present before testing and can be assessed through patient history, physical examination, or risk scores.
- 📈 The Wells score is a tool for assessing the risk of pulmonary embolism based on clinical features and risk factors.
- 🧬 D-dimer blood tests and CT angiography are common diagnostic tests for pulmonary embolism.
- 🔍 Sensitivity of a test measures its ability to correctly identify those with the disease (true positives) and is useful for ruling out diseases.
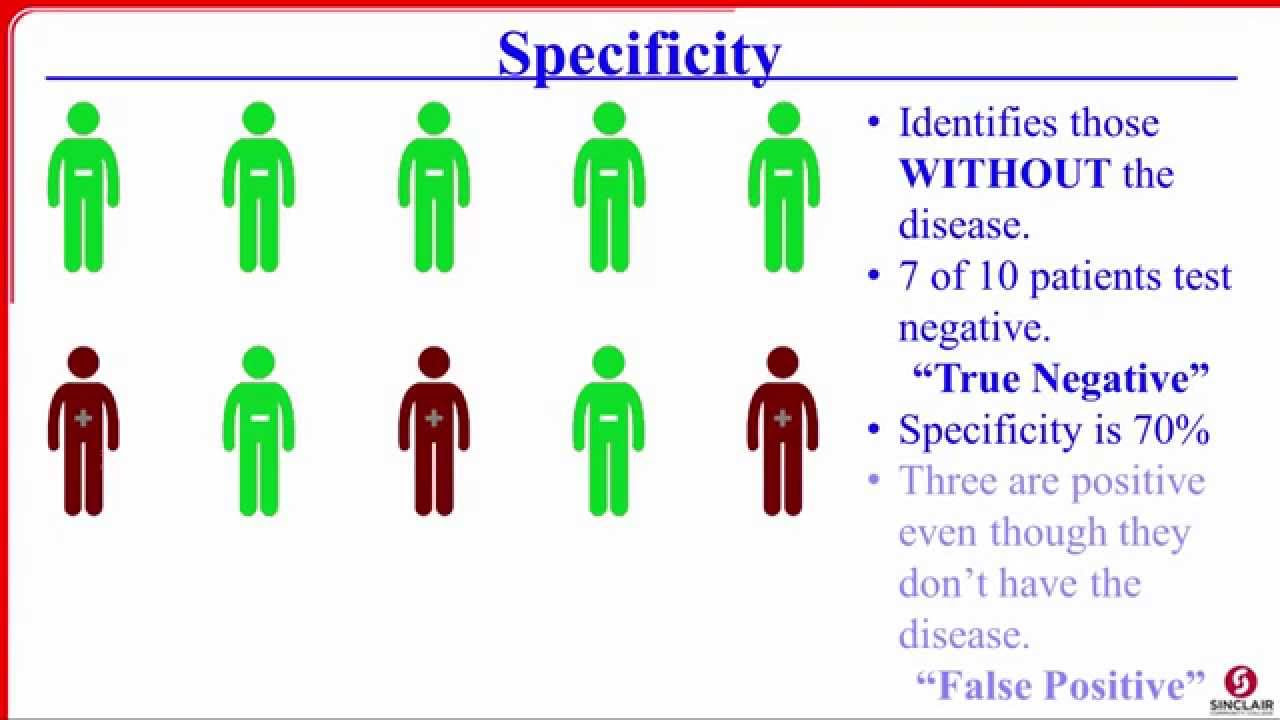
- 🎯 Specificity measures a test's ability to correctly identify those without the disease (true negatives) and is crucial for confirming a diagnosis.
- 🔢 Positive and negative predictive values help interpret the likelihood of having or not having a disease based on test results.
- 🏆 Accuracy of a diagnostic test indicates the percentage of correct results and is a measure of the test's overall correctness.
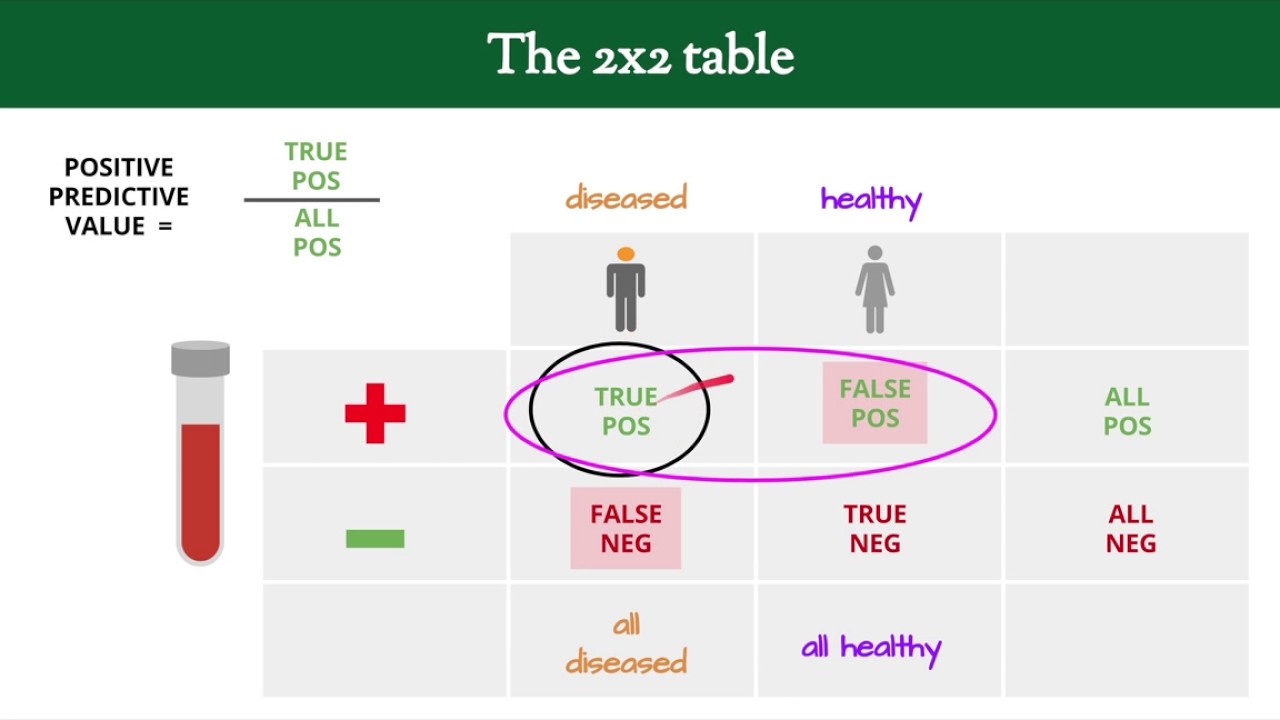
- 📝 A 2x2 table is used to present results from diagnostic studies, showing true positives, false positives, true negatives, and false negatives.
- 🚫 A negative D-dimer test, due to its high sensitivity, can confidently rule out pulmonary embolism, leading clinicians to consider other causes for symptoms.
Q & A
What are the primary learning goals of the video?
-The primary learning goals are to understand how to interpret different diagnostic testing parameters and to comprehend why clinical tests are used in practice.
What is the most probable clinical diagnosis for a 50-year-old man with breathing-dependent chest pain and a history of deep vein thrombosis?
-The most probable clinical diagnosis is pulmonary embolism.
What are the main purposes of using diagnostic tests in clinical practice?
-Diagnostic tests are used to clarify the cause of symptoms, support therapeutic decisions, assess disease severity and patient prognosis, evaluate the course of the disease and the body's response to therapy, and for disease screening.
What are examples of diagnostic tests used in clinical practice?
-Examples include imaging tests like X-rays or ultrasounds, and laboratory tests such as blood or urine tests.
What does pretest probability refer to in the context of diagnostic testing?
-Pretest probability refers to the likelihood that a disease is present before a diagnostic test is performed, which can be assessed based on history taking, physical examination, or application of a validated risk score.
How is the Well score used to determine the pretest probability of pulmonary embolism?
-The Well score assigns points to several symptoms and risk factors, and the total score is used to assess a patient's risk of having a pulmonary embolism; a score higher than four points indicates a high risk.
What are the two commonly used diagnostic tests to diagnose pulmonary embolism?
-A D-dimer blood test, which measures a small protein fragment resulting from the degradation of blood clots, and CT angiography are commonly used.
How is sensitivity defined in diagnostic tests?
-Sensitivity refers to the proportion of patients with a disease who were correctly identified by a test, also known as true positive results.
How is specificity defined in diagnostic tests?
-Specificity refers to the proportion of those who do not have the disease and have a negative test, also known as true negative results.
What does a high sensitivity test imply for ruling out a disease?
-A test with high sensitivity is very useful to rule out a disease; if the test is negative, we can be confident that the patient does not have the suspected disease.
What does a high specificity test imply for confirming a disease?
-A test with high specificity is very useful to confirm a disease; if the test is positive, we can be very sure that the patient has the suspected disease.
What is the accuracy of a diagnostic test and how is it calculated?
-Accuracy is defined as the percentage of correct test results out of all tests, calculated by the sum of true positive and true negative values, divided by the sum of all values.
What did the negative D-dimer test result indicate for the patient in the example?
-The negative D-dimer test result indicated that the doctor could confidently rule out a pulmonary embolism as the cause of the patient's symptoms.
Outlines
🧬 Introduction to Diagnostic Testing and Clinical Application
This paragraph introduces the learning objectives of the video, focusing on understanding diagnostic testing parameters and their clinical application. It presents a scenario involving a 50-year-old man with chest pain and a history of deep vein thrombosis, leading to a probable diagnosis of pulmonary embolism. The importance of diagnostic tests in clinical practice is highlighted, including their role in clarifying symptom causes, supporting therapeutic decisions, assessing disease severity and prognosis, monitoring disease progression, and screening for diseases. The paragraph also explains the concept of pre-test probability, which is assessed before performing a diagnostic test and can be determined through patient history, physical examination, or risk scores. The Wells score is introduced as a tool for assessing the risk of pulmonary embolism, and the use of D-dimer blood tests and CT angiography for diagnosis is discussed, emphasizing the need to understand the accuracy of such tests.
🔍 Understanding Diagnostic Parameters: Sensitivity, Specificity, and Predictive Values
This paragraph delves into the diagnostic parameters such as sensitivity, specificity, predictive values, and accuracy. It explains that high sensitivity tests are useful for ruling out diseases, as they detect most patients with the disease, while high specificity tests are valuable for confirming a disease's presence. The concept of predictive values is introduced, with positive predictive value indicating the likelihood of having the disease if the test is positive, and negative predictive value indicating the likelihood of not having the disease if the test is negative. The paragraph uses the rapid D-dimer test as an example to illustrate the calculation and interpretation of these parameters. It concludes with a discussion on the accuracy of diagnostic tests, which reflects the percentage of correct diagnoses based on test results. The example provided shows how the D-dimer test's results can be interpreted in clinical practice, with a focus on the implications of a negative D-dimer test in ruling out pulmonary embolism.
Mindmap
Keywords
💡Diagnostic Testing Parameters
💡Clinical Tests
💡Pulmonary Embolism
💡Pretest Probability
💡Sensitivity
💡Specificity
💡Predictive Values
💡Accuracy
💡Diagnostic Studies
💡2x2 Table
💡D-Dimer Test
Highlights
The learning goal is to interpret and understand different diagnostic testing parameters.
Clinical tests are used to clarify symptoms, support therapeutic decisions, assess disease severity and prognosis, and for disease screening.
Diagnostic tests can be performed in parallel or sequentially, with sequential testing guided by the results of the initial test.
Pre-test probability is the likelihood of a disease being present before a diagnostic test is conducted, assessed through history, physical examination, or risk scores.
The Wells score is a tool used to assess the risk of pulmonary embolism based on clinical features and risk factors.
A D-dimer blood test and CT angiography are common diagnostic tests for pulmonary embolism.
Diagnostic parameters such as sensitivity, specificity, predictive values, and accuracy are obtained via diagnostic studies.
Sensitivity refers to the proportion of true positive results among those with the disease, indicating a test's ability to rule out a disease.
Specificity is the proportion of true negative results among those without the disease, indicating a test's ability to rule in a disease.
Positive predictive value describes the probability of having the disease if the test is positive, while negative predictive value describes the probability of not having the disease if the test is negative.
Accuracy is the percentage of correct test results out of all tests, indicating the likelihood of a correct diagnosis based on the test result.
In the example, a negative D-dimer test result due to its high sensitivity allows the doctor to rule out pulmonary embolism.
The Wells score, D-dimer test, and CT angiography are used in a stepwise approach to diagnose pulmonary embolism.
Understanding pre-test probability and diagnostic test parameters is crucial for accurate clinical decision-making.
Diagnostic accuracy studies involve performing both the index test and the reference test on patients to obtain accurate parameters.
A 2x2 table is used to present results from diagnostic studies, showing true positives, false positives, true negatives, and false negatives.
Mnemonics like 'snout' for sensitivity to rule out and 'spin' for specificity to rule in help clinicians remember the implications of these parameters.
Transcripts
5.0 / 5 (0 votes)
Thanks for rating: