Peritoneal Dialysis
TLDRThe video script discusses peritoneal dialysis, a treatment for patients with kidney dysfunction. It compares peritoneal dialysis with hemodialysis, highlighting that the choice between the two depends on the individual patient's condition and circumstances. The video outlines the indications for peritoneal dialysis, such as the patient's ability to undergo surgery for vascular access, their stability concerning chronic infections or unstable hypertension, and their desire for independence and mobility. The process of peritoneal dialysis is explained, involving the use of the peritoneum as a semi-permeable membrane to filter waste using a sterile solution. The script also covers the steps for nurses during the procedure, potential complications like infections and hyperglycemia, and emphasizes the importance of patient education on the correct technique for attaching, disconnecting, and cleaning to prevent infections. The video aims to inform and prepare patients for peritoneal dialysis, ensuring they understand the process and how to manage their care.
Takeaways
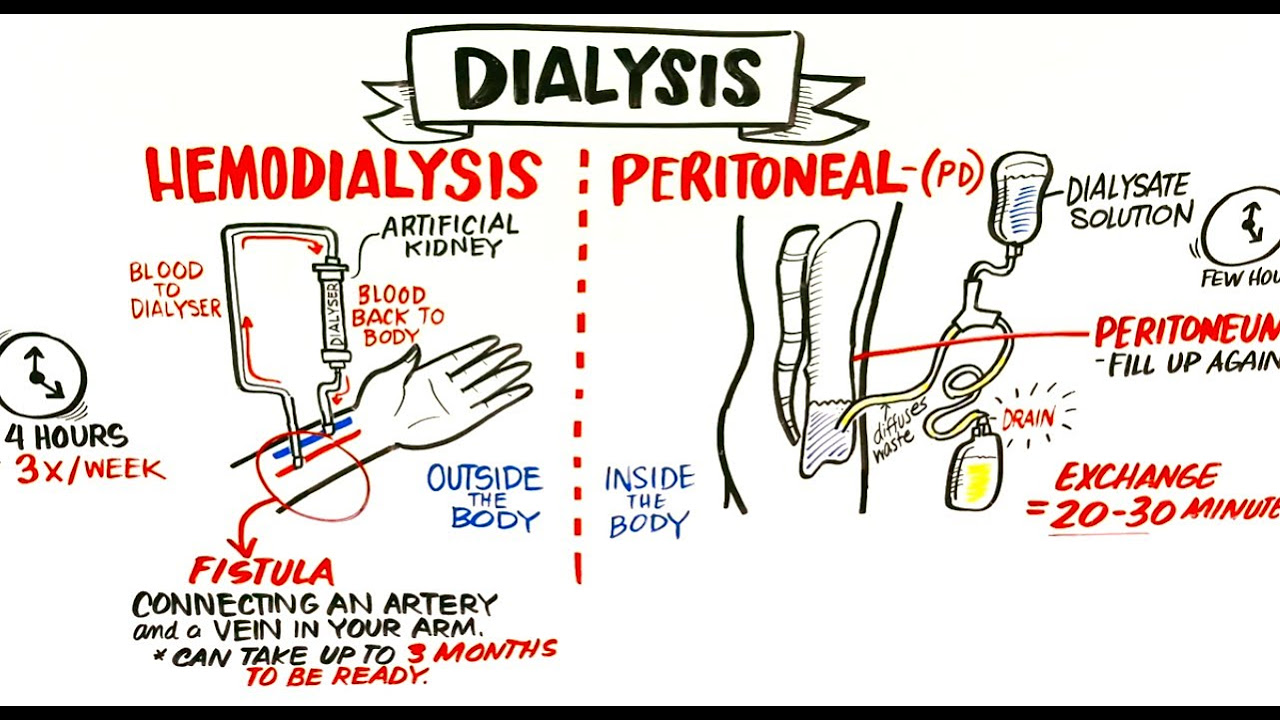
- 🔍 **Peritoneal Dialysis (PD) vs. Hemodialysis (HD):** Both are treatment options for patients with kidney dysfunction, and the choice depends on the individual patient's condition and ability to handle the procedures.
- ⏱️ **Time to Treatment:** PD can be initiated sooner than HD because it does not require waiting for a fistula or graft to heal post-surgery.
- 💡 **Patient Stability:** PD might be preferred for patients with chronic infections or unstable hypertension where HD could cause complications.
- 🏠 **Independence:** PD allows patients to maintain a level of independence and can be done at home, unlike HD which often requires visits to a facility.
- 🧴 **Peritoneum as Filter:** PD uses the peritoneum, a semi-permeable membrane in the abdominal cavity, to filter waste from the blood through a sterile dialysis solution.
- 🩺 **Peritoneal Catheter:** A catheter is surgically placed for PD, which allows for immediate use post-surgery without a long healing period.
- 🔄 **Dialysate Solution:** The process involves filling the abdomen with dialysate, allowing it to dwell, and then draining it to collect waste, using gravity without the need for machines.
- 📏 **Dry Weight:** A patient's dry weight is determined before starting PD, which is their weight without any dialysis solution in their body.
- 🔁 **Types of PD:** There are two types - Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD), with CAPD being continuous and APD typically done at night with a machine.
- 📋 **Procedure Steps:** The process includes pre-procedure checks, intra-procedure monitoring for leaks and stability, and post-procedure education on catheter care and signs of complications.
- 🚨 **Complications:** Infections, particularly around the catheter site or peritonitis, and hyperglycemia due to the hypertonic dialysate solution are key concerns with PD.
- 🧼 **Patient Education:** Emphasizes the importance of proper cleaning techniques around the catheter, aseptic connection procedures, and monitoring for signs of infection or hyperglycemia.
Q & A
What is the main topic of the video?
-The video is primarily about peritoneal dialysis, discussing its indications, setup, procedure, and considerations for patients with kidney dysfunction.
Why might a patient choose peritoneal dialysis over hemodialysis?
-A patient might choose peritoneal dialysis if they cannot handle the in-depth surgery required for hemodialysis, if they have chronic infections or unstable hypertension, or if they value the independence and flexibility it offers for home treatment.
How does the peritoneum function in peritoneal dialysis?
-The peritoneum acts as a semi-permeable membrane that allows for the instillation of a sterile solution. Filtration occurs, collecting waste, which can then be expelled into a drainage bag.
What are the two types of peritoneal dialysis mentioned in the video?
-The two types of peritoneal dialysis mentioned are continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD).
What is the significance of the 'dwell time' in peritoneal dialysis?
-The dwell time refers to the period during which the dialysate solution remains in the peritoneal cavity, allowing for the filtration process to occur and waste products to be collected.
How does the procedure for peritoneal dialysis differ between the first treatment and subsequent treatments?
-During the first treatment, dialysate is instilled and allowed to dwell before draining. For subsequent treatments, the waste is drained first, followed by the instillation of fresh dialysate and another dwell period.
What are some pre-procedure steps a nurse should take before starting peritoneal dialysis?
-Pre-procedure steps include checking the patient's weight, labs, blood sugar, ensuring informed consent, assessing the vascular access and catheter, and understanding the type of peritoneal dialysis the patient will use.
What are the key considerations during the intra-procedure phase of peritoneal dialysis?
-Key considerations include monitoring for leakage, ensuring stable vital signs, educating the patient on proper technique, and checking for signs of infection or other complications.
What are the potential complications associated with peritoneal dialysis?
-Potential complications include infections, particularly around the catheter site or peritonitis, and hyperglycemia due to the hypertonic nature of the dialysate solution.
Why is it important to check a patient's blood sugar levels during peritoneal dialysis?
-Checking blood sugar levels is important because the hypertonic dialysate can cause hyperglycemia, leading to symptoms such as dizziness or feeling unwell, which can be easily managed if detected.
What are the main points of patient education regarding peritoneal dialysis?
-Patient education should focus on understanding the setup, recognizing signs and symptoms of complications, proper attachment and disconnection techniques, cleaning and maintaining the catheter site, and the importance of aseptic technique to prevent infections.
How can a patient increase their independence with peritoneal dialysis compared to hemodialysis?
-Peritoneal dialysis allows patients to perform treatments at home, without the need for frequent visits to a medical facility, and offers flexibility to carry out daily activities, thus increasing their independence.
Outlines
🧼 Introduction to Peritoneal Dialysis
The first paragraph introduces the topic of peritoneal dialysis, contrasting it with hemodialysis as alternative treatments for patients with kidney dysfunction. It discusses patient-specific factors that might make peritoneal dialysis a preferable choice, such as the ability to avoid the six-month waiting period for vascular access maturation in hemodialysis, patient stability regarding chronic infections or unstable hypertension, and the potential for greater independence and mobility. The paragraph also explains the basic mechanism of peritoneal dialysis, using the peritoneum as a semi-permeable membrane to filter waste through the instillation and drainage of a sterile solution called dialysate.
📈 Peritoneal Dialysis Procedure and Patient Teaching
The second paragraph delves into the procedural aspects of peritoneal dialysis, outlining the steps nurses take before, during, and after the procedure. It emphasizes the importance of pre-procedure checks, including the patient's weight, labs, blood sugar, and dry weight, as well as obtaining informed consent and assessing the vascular access. The types of peritoneal dialysis, CAPD (Continuous Ambulatory Peritoneal Dialysis) and APD (Automated Peritoneal Dialysis), are explained, focusing on their operational mechanisms, patient independence, and mobility. Intra-procedure care involves monitoring for leakage, stability, and educating the patient on proper technique, while post-procedure care ensures the patient understands self-care, catheter cleaning, and signs of complications like infections.
🚨 Complications and Patient Education in Peritoneal Dialysis
The third paragraph addresses potential complications associated with peritoneal dialysis, including infections around the catheter site and peritonitis, which is a serious concern due to the risk of the patient's peritoneum becoming inflamed. It also mentions hyperglycemia as a possible complication due to the hypertonic nature of the dialysate. The paragraph concludes with a discussion on patient education, stressing the importance of proper catheter care, aseptic technique, and the recognition of signs and symptoms that require medical attention. The goal is to empower patients to manage their condition effectively and independently.
Mindmap
Keywords
💡Peritoneal Dialysis
💡Hemodialysis
💡Peritoneum
💡Dialysate
💡Continuous Ambulatory Peritoneal Dialysis (CAPD)
💡Automated Peritoneal Dialysis (APD)
💡Peritoneal Catheter
💡Dwelling Time
💡Infection
💡Peritonitis
💡Hyperglycemia
Highlights
Peritoneal dialysis is an alternative treatment for patients with kidney dysfunction, alongside hemodialysis.
The choice between peritoneal dialysis and hemodialysis is patient-specific, with no clear superiority of one over the other.
Peritoneal dialysis may be preferred when a patient cannot wait for vascular access to heal, which can take up to six months.
Stable patients with chronic infections or unstable hypertension might find peritoneal dialysis more suitable than hemodialysis.
Peritoneal dialysis allows for greater patient independence and does not require frequent visits to a facility.
The peritoneum acts as a semi-permeable membrane for filtration during peritoneal dialysis.
A peritoneal catheter is placed during surgery, enabling immediate use for dialysis without a long healing period.
Gravity is used in peritoneal dialysis, eliminating the need for machines to pump fluids.
Patients are taught proper dialysis technique, including how to handle and set up the dialysis equipment.
Two types of peritoneal dialysis are continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD).
CAPD is performed multiple times a day and allows for patient mobility, while APD is done overnight with a machine.
Intra-procedure monitoring includes checking for leaks, stable vital signs, and educating the patient on dialysis care.
Post-procedure care involves ensuring the patient understands how to maintain their catheter site and monitor for signs of infection.
Infections, particularly around the catheter site, are a significant concern and can lead to peritonitis.
Hyperglycemia is a potential complication due to the hypertonic nature of the dialysate used in peritoneal dialysis.
Proper patient education on catheter care, recognizing complications, and maintaining blood sugar levels is crucial.
Aseptic technique is essential for connecting and disconnecting dialysis equipment to prevent infections.
The video concludes with a summary of the importance of peritoneal dialysis, its setup, and patient education for successful treatment.
Transcripts
Browse More Related Video

Renal Replacement Therapy: Hemodialysis vs Peritoneal Dialysis, Animation
Failing Kidneys and Different Treatment Options

Hemodialysis

As the End Nears: Dying With Kidney Failure

Dialysis Patients and Their Machine Settings - Why Sodium Profiles Matter; Conductivity Profiles

Queen of dialysis describes her dependence on a machine | Maddy Warren | TEDxRoyalTunbridgeWells
5.0 / 5 (0 votes)
Thanks for rating: