Neonatal Resuscitation Education for Essential Providers
TLDRThe transcript outlines the critical communication and preparedness required for obstetric and newborn care providers during delivery. It emphasizes the importance of having necessary personnel and equipment, and knowing the plan for cord clamping and neonatal resuscitation. The script details a scenario where providers must act swiftly to address a newborn's poor respiratory effort, using positive pressure ventilation (PPV) and corrective measures to stimulate the baby's breathing and increase heart rate. The focus is on the foundational skills of PPV and the necessity of a well-coordinated team for neonatal resuscitation.
Takeaways
- 🤝 Effective communication is crucial among healthcare providers before every birth to coordinate care and ensure readiness.
- 💬 Ask and be aware of the necessary personnel and equipment for every delivery to manage any situation effectively.
- 🚑 Be prepared to handle risk factors and have a plan for neonatal resuscitation if needed.
- 👶 Prioritize the baby's stabilization and initial steps, including positive pressure ventilation, for every delivery.
- 🏥 Ensure that all supplies and equipment for complete resuscitation are readily available and that you are familiar with their use.
- 👩⚕️ At least one qualified individual should be solely responsible for the baby's stabilization at birth.
- 👥 Increase the number of qualified individuals for the baby when risk factors are present.
- 🛠️ Use the MR SOPA mnemonic for ventilation correction steps when effective ventilation is not achieved.
- 📈 Monitor the baby's heart rate as the primary indicator of effective ventilation.
- 👃 Suctioning and opening the airway can be essential steps in neonatal resuscitation.
- 🌟 Recognition of spontaneous respirations and the baby's ability to breathe on its own are positive signs of successful resuscitation.
Q & A
What is the primary goal of establishing effective communication among obstetric and newborn providers?
-The primary goal of establishing effective communication among obstetric and newborn providers is to better coordinate care before every birth, ensuring the necessary personnel and equipment are available for a smooth delivery process.
What are the four key questions providers should ask to prepare for a delivery?
-The four key questions providers should ask include: 1) Is the fluid clear? 2) Are there any other risk factors to be aware of? 3) What is the plan for cord clamping? 4) How to handle any issues that may arise during the delivery.
What is the significance of knowing the baby's gestational age in terms of initial oxygen concentration requirements?
-Knowing the baby's gestational age is significant because it helps determine the appropriate initial oxygen concentration. For babies at 35 weeks gestation or greater, the starting oxygen concentration should be 21%, while for those less than 35 weeks, it should be between 21% and 30%.
What is the role of a qualified individual in the stabilization of a baby at delivery?
-A qualified individual is solely responsible for the stabilization of the baby at delivery and is skilled in the initial steps, including giving positive pressure ventilation (PPV) to support the baby's respiratory efforts if needed.
What should be the team composition for deliveries with identified risk factors that increase the likelihood of neonatal resuscitation?
-For deliveries with identified risk factors that increase the likelihood of neonatal resuscitation, two qualified individuals should be present solely for the baby. Additionally, a qualified team with full resuscitation skills should be immediately available if more advanced measures are required.
How is the effectiveness of ventilation determined during neonatal resuscitation?
-The effectiveness of ventilation is determined primarily by a rising heart rate. After 15 seconds of effective PPV, the heart rate should be on the rise. If the heart rate is increasing, continue PPV until it is determined that the baby no longer needs it.
What are the initial peak inspiratory pressure (PIP) settings for PPV based on the baby's gestational age?
-The initial PIP settings for PPV should start between 20 and 25 centimeters of water, with the pressure determined by how hard the bag is squeezed.
How can chest movement be assessed during PPV?
-Chest movement can be assessed visually or by gently feeling for a rise and fall of chest movement with your hand. This helps to determine if the ventilation is effectively moving the chest and reaching the lungs.
What is the Mr. SOPA mnemonic and how is it used in neonatal resuscitation?
-Mr. SOPA is a mnemonic that stands for Mask adjustment, Reposition the airway, Suction mouth and nose, Open the mouth, Pressure increase, and Alternative Airway. It is used to remember the six ventilation correction steps to take when ineffective ventilation is determined.
What actions should be taken if chest rise and heart rate increase are not observed after 30 seconds of PPV?
-If chest rise and heart rate increase are not observed after 30 seconds of PPV, corrective measures should be taken immediately. This includes using the Mr. SOPA steps to adjust the mask, reposition the airway, suction the mouth and nose, ensure the mouth stays open, increase pressure cautiously, and consider alternative airways if necessary.
What is the most important and effective step in neonatal resuscitation?
-The most important and effective step in neonatal resuscitation is the ventilation of the newborn's lungs. Learning how to provide positive pressure ventilation (PPV) is the foundation of neonatal resuscitation.
Outlines
👶 Effective Communication and Preparation for Neonatal Resuscitation
This paragraph emphasizes the importance of establishing effective communication among obstetric and newborn care providers to coordinate care efficiently. It outlines the necessity of being prepared with the right personnel and equipment for every birth. The discussion includes a scenario where providers go through a checklist of questions to ensure they have a clear understanding of the situation, including any risk factors and plans for cord clamping. The paragraph also stresses the need for a qualified individual to be solely responsible for the baby's stabilization at birth and the presence of skilled personnel for initial steps like positive pressure ventilation. It further explains the preparation and use of supplies and equipment, the importance of a team with full resuscitation skills, and the initial steps in neonatal resuscitation, including the critical role of positive pressure ventilation (PPV) in stimulating the newborn's lungs.
🚑 Advanced Neonatal Resuscitation Techniques and Troubleshooting
The second paragraph delves into the advanced techniques and troubleshooting steps involved in neonatal resuscitation. It begins with a scenario where the newborn is not breathing well, and the healthcare provider decides to stimulate the baby and consider clamping the cord. The paragraph outlines the importance of monitoring the newborn's heart rate and the initial steps to take if the baby is not responding well. The paragraph introduces the mnemonic 'MR SOPA' to remember the six ventilation correction steps when effective ventilation is not achieved. These steps include mask adjustment, suctioning, opening the airway, increasing pressure, considering alternative airways like a laryngeal mask airway (LMA), and reassessing after each step. The summary highlights the process of suctioning, increasing pressure, and the successful use of an LMA as an alternative airway, which leads to observable chest rise, an increasing heart rate, and the baby's spontaneous respirations. The paragraph concludes with the baby showing signs of improvement, starting to breathe on its own, and crying, indicating a successful resuscitation effort.
Mindmap
Keywords
💡Effective Communication
💡Risk Factors
💡Initial Resuscitation
💡Positive Pressure Ventilation (PPV)
💡Heart Rate
💡Chest Movement
💡Neonatal Resuscitation
💡Laryngeal Mask Airway (LMA)
💡MRSOPA
💡Advanced Resuscitation
💡Spontaneous Respirations
Highlights
Establishing effective communication is crucial for coordinating care before every birth.
Asking four key questions helps determine the necessary personnel and equipment for a delivery.
It's important to assess the fluidity and clarity of amniotic fluid during delivery.
Identifying any additional risk factors ensures a safer delivery process.
Delayed cord clamping can be implemented if there are no reasons to stop it.
Preparation for initial resuscitation includes having all necessary supplies and equipment ready.
At least one qualified individual should be responsible for the baby's stabilization at birth.
Two qualified individuals should be present for the baby when any risk factor is identified.
A team with full resuscitation skills should be immediately available if advanced measures are required.
Ventilation of the newborn's lungs is the most important step in neonatal resuscitation.
Initial peak inspiratory pressure (PIP) should start between 20 and 25 centimeters of water.
Effective ventilation can be indicated by a rising heart rate within 15 seconds.
Chest movement assessment is crucial for determining the effectiveness of ventilation.
MR SOPA is a mnemonic for remembering the six ventilation correction steps.
An alternative airway, such as an LMA, can be used if chest rise and heart rate do not improve.
Continuous reassessment and adjustments ensure effective neonatal resuscitation.
The baby's spontaneous respirations and crying indicate successful resuscitation.
Transcripts
Browse More Related Video

Mock Code Training Video

Respiratory Distress: ABC Assessment , Diagnosis & Examination – Emergency Medicine | Lecturio
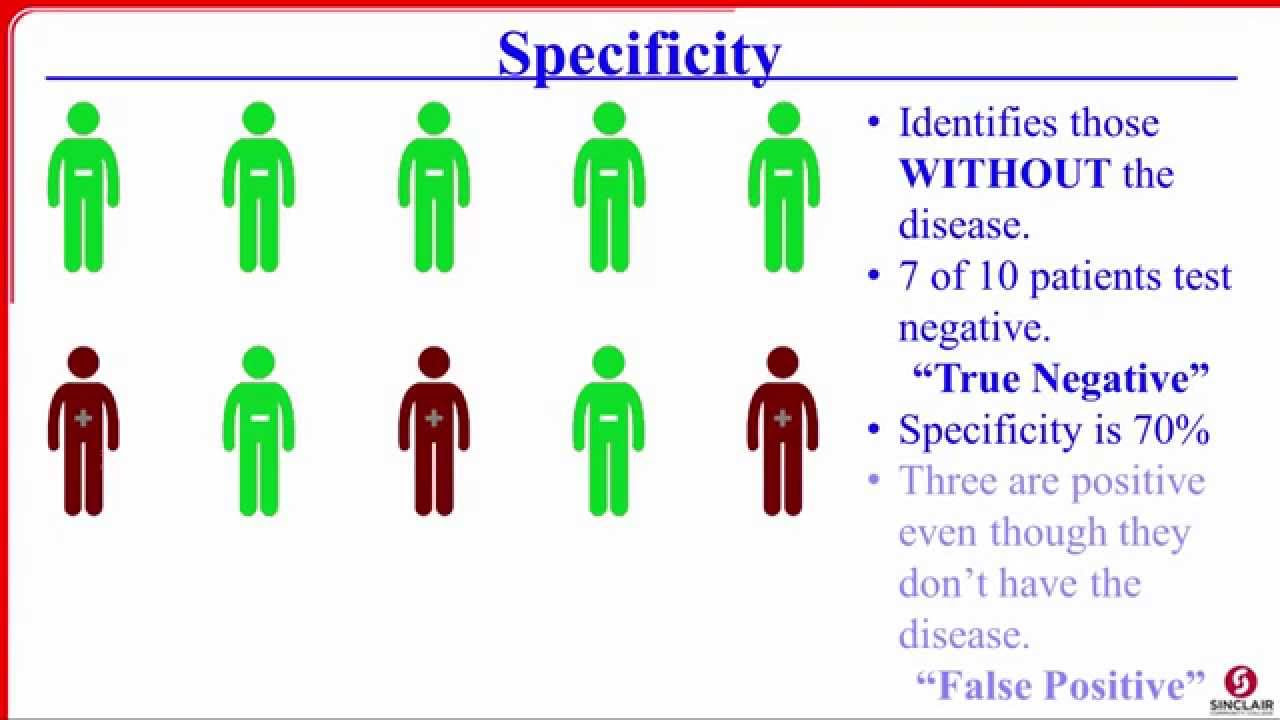
Sensitivity, Specificity, PPV, and NPV

Trauma: Primary Survey, ABCDE-Assessments & Take-home points – Emergency Medicine | Lecturio

Physical Examination of a Premature Infant

This Doctor Wants to Humanize Death | Op-Docs
5.0 / 5 (0 votes)
Thanks for rating: