Nephrolithiasis | Kidney Stones
TLDRThe video script delves into the medical condition nephrolithiasis, commonly known as kidney stones. It outlines the three-pronged system behind stone formation, emphasizing the importance of understanding the pathophysiology, diagnostics, and treatment. The discussion covers the role of urinary solvents, stone inhibitors, and solutes in the formation of different types of kidney stones, including calcium oxalate, calcium phosphate, struvite, uric acid, and cysteine stones. The script also addresses the complications of kidney stones, such as renal colic and urinary tract infections, and the potential for acute kidney injury and sepsis. Diagnostic methods like CT scans, ultrasounds, and urinalysis are highlighted, along with treatments ranging from pain management and medical expulsive therapy to surgical interventions like ureteroscopy and percutaneous nephrolithotomy (PCNL). The importance of patient education on hydration, diet, and medication adherence is underscored to prevent future occurrences.
Takeaways
- 💠 **Understanding Nephrolithiasis**: Nephrolithiasis, or kidney stones, can be understood through a three-prong system involving less urinary solvent, fewer stone inhibitors, and an increase in urinary solutes.
- 💧 **Dehydration and Solvent**: Dehydration leads to a decrease in urinary solvent, which increases the risk of solute supersaturation, precipitation, and crystal formation.
- 🚫 **Stone Inhibitors**: A decrease in stone inhibitors, such as urinary citrate and pH levels, can lead to an increase in solute precipitation and stone formation.
- 🔍 **Urinary pH Impact**: Urinary pH plays a crucial role in stone formation, with high pH associated with calcium phosphate and struvite stones, and low pH with uric acid and cysteine stones.
- 🔑 **Citrate's Role**: Low urinary citrate levels can increase the risk of calcium oxalate stones by allowing more calcium to bind with oxalate instead.
- 📈 **Solute Overload**: An increase in urinary solutes like calcium, uric acid, oxalate, and cysteine can lead to supersaturation and stone formation.
- 😖 **Symptoms and Complications**: Kidney stones can cause severe pain, urinary tract symptoms, and complications like hydronephrosis, acute kidney injury, and pyelonephritis.
- 🩺 **Diagnostic Approach**: Diagnosis of nephrolithiasis typically involves imaging studies like CT scans, ultrasound, or KUB X-rays, and urinalysis to determine the type of stone.
- 🛑 **Emergent Treatment**: In cases of acute kidney injury, pyelonephritis, or uncontrollable pain, emergent treatment may include ureteral stents or percutaneous nephrostomy tubes.
- 💊 **Medical Management**: For non-emergent cases, treatment may involve pain control, anti-emetics, IV fluids, and medications like tamsulosin to help stones pass.
- ⚕️ **Long-term Prevention**: Long-term management focuses on addressing the underlying causes, such as dietary changes, increased fluid intake, and medication adjustments to prevent future stone formation.
Q & A
What is the basic concept of nephrolithiasis?
-Nephrolithiasis is a condition where hard deposits of mineral and acid salts, known as stones, form in the urinary tract. The basic concept involves a three-prong system that includes a decrease in urinary solvent, a decrease in stone inhibitors, and an increase in urinary solutes, which together can lead to stone formation.
Why does dehydration increase the risk of nephrolithiasis?
-Dehydration leads to a decrease in urinary solvent, which increases the concentration or saturation of solutes in the urine. This super saturation can cause solutes to precipitate out of the solution, leading to crystal formation and eventually the development of kidney stones.
How does urinary pH influence the formation of different types of kidney stones?
-Urinary pH plays a significant role in stone formation. Low urinary pH increases the risk of uric acid and cysteine stones, while high urinary pH can lead to the formation of calcium phosphate and struvite stones. The pH level can affect the solubility of certain substances in the urine, influencing whether they precipitate out to form stones.
What is the role of citrate in preventing kidney stone formation?
-Citrate is a stone inhibitor that helps bind with calcium, reducing the amount of free calcium available to bind with oxalate and form calcium oxalate stones. A low level of urinary citrate can increase the risk of calcium oxalate stone formation.
What are the common symptoms associated with kidney stones?
-Common symptoms of kidney stones include flank pain that may radiate to the groin, renal colic characterized by intermittent intense pain, nausea and vomiting, urinary tract infection-like symptoms if the stone is near the ureterovesical junction (UVJ), and potentially hematuria or blood in the urine.
What are the potential complications of kidney stones if left untreated?
-Untreated kidney stones can lead to serious complications such as hydronephrosis (enlargement of the kidney due to urine backup), acute kidney injury, urinary stasis, pyelonephritis (kidney infection), and urosepsis, which is a life-threatening condition.
How can medical therapy help in the treatment of kidney stones less than 10 millimeters in size?
-Medical therapy can be effective for smaller stones by using pain control medications like NSAIDs or opioids, anti-emetics for nausea and vomiting, IV fluids to prevent dehydration, and potentially alpha-blockers like tamsulosin to help relax the ureter and facilitate stone passage.
What diagnostic imaging methods are used to detect kidney stones?
-The gold standard for detecting kidney stones is a CT scan of the abdomen and pelvis. Other imaging methods include renal ultrasound, which is useful for minimizing radiation exposure in children or pregnant women, and a KUB (Kidney, Ureter, Bladder) X-ray, which can provide hints about the stone type based on its radio-opacity or radio-lucency.
What is the significance of urine microscopy in the evaluation of kidney stones?
-Urine microscopy is important as it can reveal the presence of red blood cells (indicating hematuria), white blood cells (suggestive of infection), and various crystal shapes which can help identify the type of kidney stone. Different stone types have characteristic crystal shapes that can be seen under a microscope.
How does the size and location of a kidney stone influence the choice of treatment?
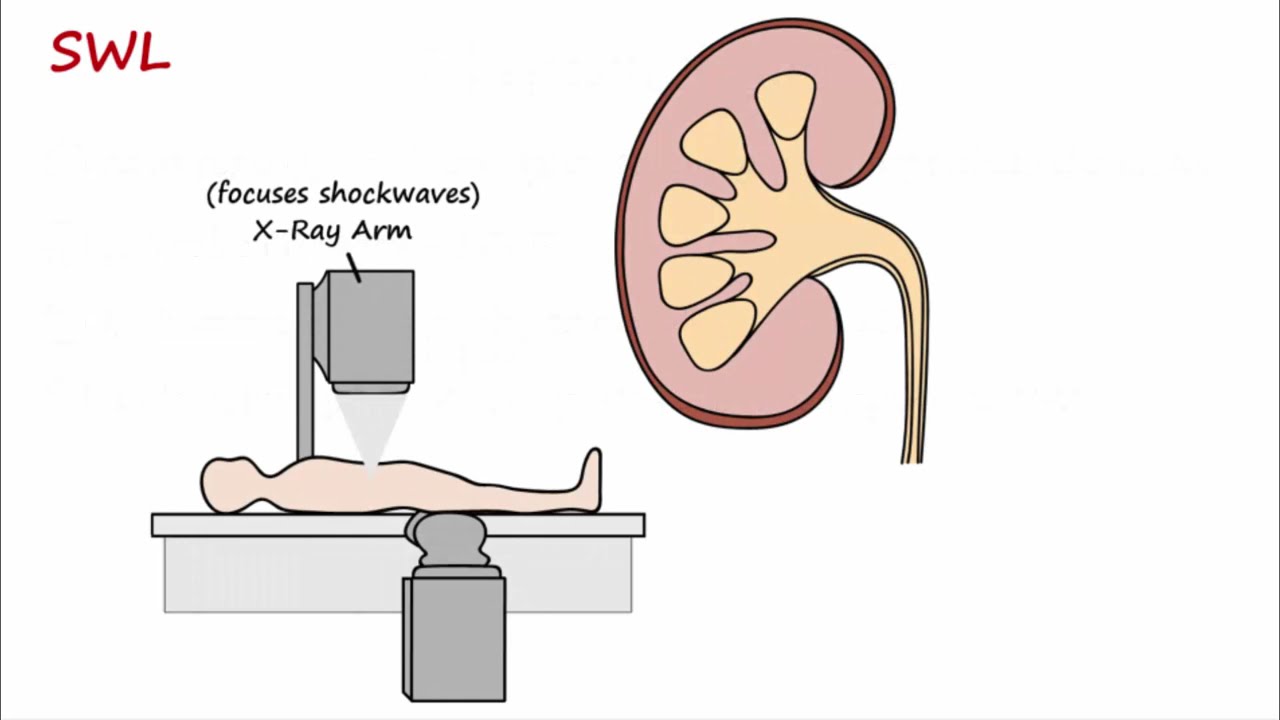
-The size and location of a kidney stone greatly influence the treatment approach. Stones less than 10 millimeters may pass spontaneously with medical therapy. For stones greater than 10 millimeters, especially in the mid-distal ureter, extracorporeal shock wave lithotripsy (ESWL) or ureteroscopy with lithotripsy is preferred. For stones greater than 20 millimeters or staghorn calculi, percutaneous nephrolithotomy (PCNL) is often performed.
What are some long-term management strategies to prevent recurrent kidney stone formation?
-Long-term management strategies include ensuring adequate hydration, dietary modifications to reduce sodium, protein, and oxalate intake, use of medications like thiazide diuretics to increase calcium reabsorption, allopurinol to reduce uric acid formation, and potassium citrate to alkalinize urine. Treating underlying conditions like gout, hyperparathyroidism, or malignancy is also crucial.
Outlines
🎬 Introduction to Nephrolithiasis
The video begins with an introduction to nephrolithiasis, a medical condition involving the formation of stones in the kidneys. The speaker encourages viewers to support their content by liking, commenting, and subscribing. They also mention that additional resources such as notes and illustrations can be found on their website. The speaker outlines the basics of nephrolithiasis, explaining that it can be understood through a three-prong system involving pathophysiology, diagnostics, and treatment.
💠 The Pathophysiology of Stone Formation
The speaker delves into the pathophysiology behind nephrolithiasis, explaining the process of stone formation. They discuss the concept of urinary solvents and how a decrease in them can lead to super saturation of solutes, resulting in solute precipitation and crystal formation. The importance of stone inhibitors is highlighted, with a focus on urine pH and urinary citrate as key factors. The video also touches on the role of increased urinary solutes, such as calcium, uric acid, cysteine, and oxalate, in stone formation.
🚨 Complications of Nephrolithiasis
The video outlines the potential complications of nephrolithiasis, including ureter mucosal irritation, hematuria, urinary tract infection-like symptoms, and renal colic. It emphasizes the importance of recognizing when nephrolithiasis becomes an emergency situation, such as in cases of acute kidney injury, pyelonephritis, or uncontrollable pain and vomiting. The speaker also discusses the risk of hydronephrosis and the associated increase in capsular hydrostatic pressure that can lead to a reduced glomerular filtration rate.
🚨 Emergent Nephrolithiasis and Treatment
The speaker discusses the signs of emergent nephrolithiasis, which include acute kidney injury, pyelonephritis, and severe pain that is refractory to medical therapy. They explain the urgency of treating these conditions to prevent life-threatening complications like sepsis. The video covers emergency treatments such as ureteral stenting and percutaneous nephrostomy tube placement to alleviate obstructions and restore urine flow.
💊 Medical Management of Nephrolithiasis
The video describes the medical management of nephrolithiasis, focusing on pain control, the use of anti-emetics for nausea and vomiting, and the potential use of an alpha blocker like tamsulosin to help relax the ureter and facilitate stone passage. It emphasizes that for stones less than 10 millimeters, medical therapy is often sufficient, while larger stones may require surgical intervention.
🔍 Diagnostic Imaging for Nephrolithiasis
The speaker explains the importance of imaging in diagnosing nephrolithiasis, with a CT scan of the abdomen and pelvis being the gold standard. They also mention the use of renal ultrasound, particularly in children or pregnant women, and discuss the limitations of intravenous pyelogram and kidney, ureter, bladder (KUB) x-ray. The video highlights the KUB x-ray's ability to hint at the type of stone based on its radio-opacity or radio-lucency.
🧪 Urinalysis and Stone Type Determination
The video outlines the use of urinalysis and microscopy to determine the type of kidney stone. It discusses how the presence of red and white blood cells, bacteria, and the urine pH can provide clues to the type of stone formed. The speaker also explains how certain medications and dietary changes can help prevent stone formation by addressing the underlying causes, such as reducing sodium and protein intake, using thiazide diuretics, and treating underlying conditions like gout or malignancies.
🛠️ Long-term Management of Nephrolithiasis
The speaker concludes with the long-term management of nephrolithiasis, emphasizing the need to address the causes of stone formation. They discuss the importance of hydration, adjusting urinary pH, and treating underlying conditions. The video also mentions the use of specific medications like allopurinol for uric acid stones and TAYCRON for cysteine stones, and the role of antibiotics in treating struvite stones.
Mindmap
Keywords
💡Nephrolithiasis
💡Solvent Precipitation
💡Urinary pH
💡Citrate
💡Dehydration
💡Renal Colic
💡Acute Kidney Injury (AKI)
💡Ureteral Stent
💡Percutaneous Nephrolithotomy (PCNL)
💡Urinary Solutes
💡Urinary Tract Infection (UTI)
Highlights
The video discusses nephrolithiasis, explaining its pathophysiology, diagnostics, and treatment.
Nephrolithiasis is outlined as a three-prong system involving urinary solvent, stone inhibitors, and urinary solutes.
Dehydration increases the risk of nephrolithiasis by reducing urinary solvent and causing solute supersaturation.
A decrease in stone inhibitors like urinary citrate can lead to calcium oxalate stone formation.
An increase in urinary solutes such as calcium, uric acid, oxalate, and cysteine can cause different types of kidney stones.
The video explains that low urine pH can increase the risk of uric acid and cysteine stones, while high urine pH can lead to calcium phosphate and struvite stones.
The formation of kidney stones can cause ureteral mucosal irritation, hematuria, and urinary tract infection-like symptoms.
Renal colic, a severe flank pain that can radiate to the groin, is caused by the stretching and spasm of the ureter due to a stuck stone.
The presence of a kidney stone can lead to acute kidney injury and pyelonephritis if not treated promptly.
The video describes the complications of nephrolithiasis, including hydronephrosis and the potential for sepsis in severe cases.
Different types of kidney stones are associated with specific urine pH levels and solute compositions.
The treatment for nephrolithiasis includes pain management, addressing dehydration, and potentially surgical intervention for larger stones.
Medical therapy with drugs like tamsulosin can help small stones pass and reduce spasms in the ureter.
For larger stones that are non-responsive to medical therapy, procedures like percutaneous nephrolithotomy (PCNL) or ureteroscopy with lithotripsy are used.
The video emphasizes the importance of identifying and treating any underlying conditions that contribute to stone formation.
Diagnostic tools such as CT scans, urinalysis, and urine microscopy are crucial for determining the type of kidney stone and appropriate treatment.
Long-term management of nephrolithiasis involves lifestyle changes, dietary modifications, and medications tailored to the specific type of stone.
Transcripts
Browse More Related Video

Renal Calculi

Urinary/Kidney Stones - Overview (signs and symptoms, risk factors, pathophysiology, treatment)
Kidney Stones - Types, Formation, Treatment, Prevention

Everything You Need to Know About Urinary Stones | Caroline Wallner, MD | UCLAMDChat

Urine Crystals & Kidney Stones

Urinary Alkalinization for Kidney Stones
5.0 / 5 (0 votes)
Thanks for rating: